"LUNAR: Full Moon or Eclipse? An exploration into tumor treating fields in lung cancer"
This is the title of our new paper out in the Journal of Cancer Policy!
The LUNAR trial
Our new paper, co-authored with Vinay Prasad, is out in the Journal of Cancer Policy. It is an analysis of the LUNAR trial and raises broader questions about Tumor Treating Fields.
Tumor Treating Fields (TTFs) are a medical device therapy that uses electric fields delivered through adhesive arrays placed on patients’ skin. In the LUNAR trial, patients with metastatic non-small cell lung cancer (NSCLC) who had previously received platinum-based chemotherapy were treated with TTFs in addition to standard therapy (either checkpoint inhibitors or docetaxel). This combination led to a median survival benefit of 3.3 months.
However, the LUNAR trial has many limitations, making it of little to no value for informing current clinical practice.
Patients enrolled in LUNAR do not mirror current practice
First-line immunotherapy has been the standard of care for years. However, 68% of patients in LUNAR did not receive prior immunotherapy. Second, among patients allocated to docetaxel — likely because this “choice” was based on local availability —41% had no prior exposure to immunotherapy.
In other words, a significant proportion of patients did not receive first-line standard-of-care (immunotherapy), were enrolled in LUNAR, and again did not receive immunotherapy but docetaxel instead!
Survival analysis: p-hacking?
During LUNAR, it was decided to reduce the sample size after the Data Monitoring Committee (DMC) requested an unplanned interim analysis due to slow accrual. However, the DMC may have departed from pre-specified statistical rules. Unfortunately, even when asked for clarification. the DMC analysis remain unshared, and no explanation has been provided.
In the absence of prespecified and stated reasons to alter sample size, concern arises that the decision was influenced by a chance deviation in data that favored the intervention. It may be tempting to “quit while you are ahead”, and seek to curtail a trial trending in a favorable direction.
Why the analysis remain unshared after the end of the trial has no justification.
Survival analysis: informative censoring?
When a higher proportion of patients drop out, this may be due to increased toxicity. Then, it is plausible that frailer patients drop more easily when facing toxicity, and these same patients may be at higher risk of progressive disease or dying. This is the core concept of informative censoring. Because these patients are uncaptured, the final results may be artificially skewed.
In LUNAR, we suspect this happened, with both more dropouts and more toxicity in the TTFs group (serious adverse events occurred in 53% of patients receiving TTFs, compared to 38% in the control group).
Following a correspondence published in The Lancet Oncology with the LUNAR investigators (also available here), our concerns were confirmed: they actually shared reasons for censoring in their reply (also reply and supplement here). After excluding patients censored due to data cut-off, a 10 percentage-point higher rate of censoring was observed in the TTFs arm, mainly driven by withdrawal of consent.
We decided to explore, based on digitized curves, whether informative censoring could have affected the results. By assuming that 50% of the censored patients in the TTFs group over the first 12 months dropped out due to toxicity and would have experienced the event if not censored, the survival benefit would no longer be statistically significant. The analysis is available here: https://www.timotheeolivier-research.com/breaking-ice (select “LUNAR-OS”).
Even if only hypothesis-generating, this sensitivity analysis — combined with the sample size modification — raises questions about the reliability of the presented results.
Open-label design, and the lack of a sham-control
LUNAR was an open-label trial and not a sham-controlled study. What would a sham-controlled study look like? It would involve “false” TTFs for controls — but with the same level of care around patients.
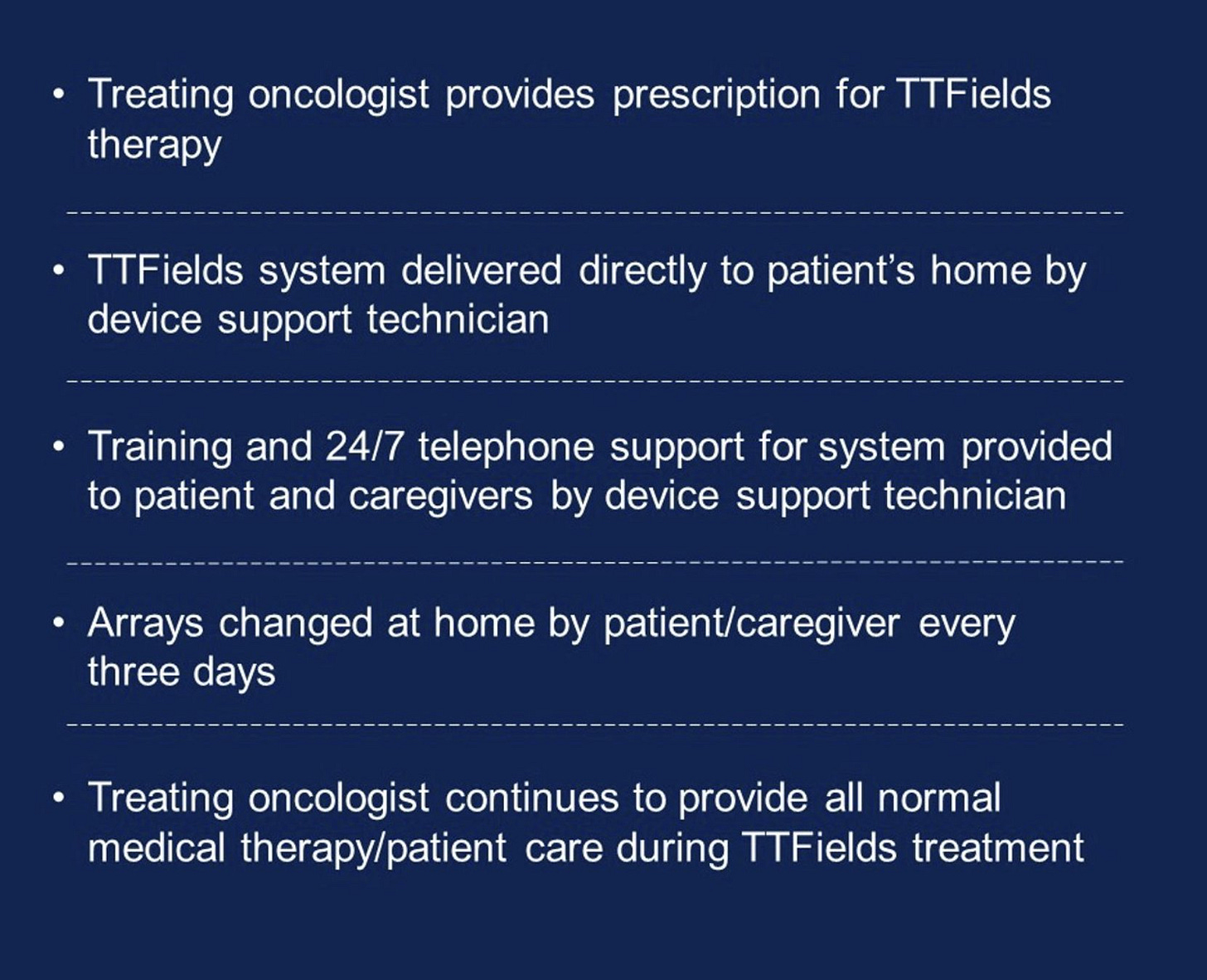
Indeed, patients in the TTFs group received a significant level of extra attention, including continuous 24/7 support, frequent home-based visits for array changes every three days, and the convenience of direct home deliveries (slide from ASCO 2023 below).
The main issue is that TTFs automatically come with “increased vigilance.” To what extent this could lead to better survival in a very poor prognosis setting is a key question. We know from a randomized trial led by Jennifer Temel that early palliative care for patients with metastatic lung cancer led to a survival gain of 2.7 months, close to the 3.3 months gain reported in LUNAR.
In the case of LUNAR — and TTFs more broadly — without sham-controlled trials, we cannot exclude that any observed survival gain is driven by the by-product of the extra vigilance associated with the device.
Final thoughts
Current data on TTFs in NSCLC have limited clinical relevance, as today’s patients differ from those enrolled in LUNAR. Several factors may have inflated the survival gain: higher censoring in the TTFs arm, reduced sample size increasing the risk of chance findings, and the lack of sham control.
A sham-controlled trial would be key in answering whether TTFs are beneficial. In the meantime, regulators should lean toward protecting poor prognosis patients who will naturally seek for more options. Those should not be exposed to procedures with significant toxicities before reaching sound confidence that they provide a clinical benefit.
Check out our visual abstract! (and full paper here)







Great review. Thanks for all your time and effort. This subject is so important.